PUBLICATIONS UPTO MAY 17th 2015
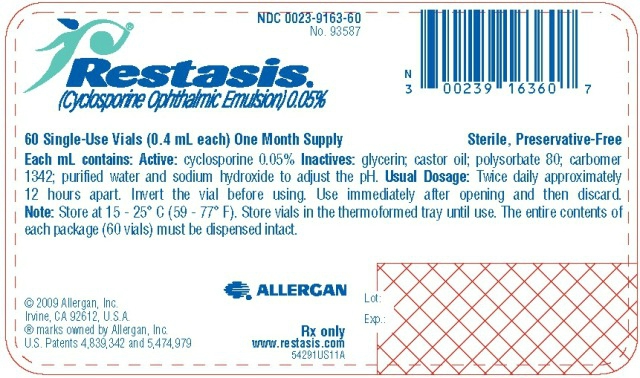
RESTASIS - cyclosporine emulsion Allergan, Inc. ---------- RESTASIS® (cyclosporine ophthalmic emulsion) 0.05% Sterile, Preservative-Free RESTASIS ® (cyclosporine ophthalmic emulsion) 0.05% contains a topical immunomodulator with anti-inflammatory effects. Cyclosporine's chemical name is Cyclo[[(E)-(2S,3R,4R)-3-hydroxy-4-methyl-2-(methylamino)-6-octenoyl]-L-2-aminobutyryl-N-methylglycyl-N-methyl-L-leucyl-L-valyl-N-methyl-L-leucyl-L-alanyl-D-alanyl-N-methyl-L-leucyl-N-methyl-L-leucyl-N-methyl-L-valyl] and it has the following structure: Structural Formula Cyclosporine is a fine white powder.
http://dailymed.nlm.nih.gov
| 1. | Drugs. 2015 May 13. [Epub ahead of print]
Author information:
Abstract
Diquafosol ophthalmic solution 3 % (Diquas®) is a P2Y2 receptor agonist that promotes tear fluid and mucin secretion and is currently approved in Japan and South Korea for the treatment of dry eye. In randomized, double-blind, multicentre trials in patients with dry eye, significantly greater improvements in fluorescein and rose bengal staining scores were seen with diquafosol ophthalmic solution 3 % than with placebo, and diquafosol ophthalmic solution 3 % was noninferior to sodium hyaluronate ophthalmic solution 0.1 % in terms of the improvement in the fluorescein staining score and more effective than sodium hyaluronate ophthalmic solution 0.1 % in terms of the improvement in the rose bengal staining score. The efficacy of diquafosol ophthalmic solution 3 % in the treatment of dry eye was maintained in the longer term, with improvements also seen in subjective dry eye symptoms, and was also shown in a real-world setting. Diquafosol ophthalmic solution 3 % also demonstrated efficacy in various specific dry eye disorders, including aqueous-deficient dry eye, short tear film break-up time dry eye, obstructive meibomian gland dysfunction, dry eye following laser in situ keratomileusis surgery and dry eye following cataract surgery, as well as in contact lens wearers and visual display terminal users. Diquafosol ophthalmic solution 3 % was generally well tolerated in patients with dry eye, with eye irritation the most commonly reported adverse event. In conclusion, diquafosol ophthalmic solution 3 % is a useful option for the treatment of dry eye. |
| PMID: 25968930 [PubMed - as supplied by publisher] | |
| Related citations | |
 |
| 2. | Clin Investig (Lond). 2015;5(3):267-285.
Author information:
Abstract
Dry eye has gained recognition as a public health problem given its high prevalence, morbidity and cost implications. Although dry eye is common and affects patients' quality of life, only one medication, cyclosporine 0.05% emulsion, has been approved by the US FDA for its treatment. In this review, we summarize the basic science and clinical data regarding the use of cyclosporine in the treatment of dry eye. Randomized controlled trials showed that cyclosporine emulsion outperformed vehicles in the majority of trials, consistently decreasing corneal staining and increasing Schirmer scores. Symptom improvement was more variable, however, with ocular dryness shown to be the most consistently improved symptom over vehicle. |
| PMID: 25960865 [PubMed] | |
| Related citations | |
| 3. | Evid Based Complement Alternat Med. 2015;2015:143858. doi: 10.1155/2015/143858. Epub 2015 Apr 16.
Author information:
Abstract
Background. The efficacy of acupuncture in dry eye syndrome patients remains controversial. Methods. Pubmed, Ovid, Cochrane libraries, CNKI, Wanfang, and CQVIP databases were electronically searched until October 1, 2014. Outcomes including tear break-up time (BUT), Schirmer I test (SIT), and cornea fluorescein staining (CFS) were analyzed. A meta-analysis was performed using both fixed- and random-effects models based on heterogeneity across studies. Results. Seven studies were included in this study; 198 and 185 patients were randomly treated with acupuncture and artificial tears, respectively. The overall BUT of patients in acupuncture group was significantly longer than that of the artificial tears group after treatment (P < 0.00001). The SIT was significantly higher in the acupuncture group than that in the artificial tears group after treatment (P = 0.001). The CFS of patients in acupuncture group was significantly improved compared to that in artificial group (P < 0.0001). Conclusions. Acupuncture therapy is effective for the dry eye patients, partly better than artificial tear treatment. |
| PMID: 25960747 [PubMed] | |
| Related citations | |
  |
| 4. | Ann Rheum Dis. 2015 Apr;74(4):e31. doi: 10.1136/annrheumdis-2014-207150. Epub 2015 Jan 14.
Risselada AP1, Hair Md2, Kruize AA3, Bijlsma JW4, van Roon JA5.
Author information:
Comment on
|
| PMID: 25589514 [PubMed - indexed for MEDLINE] | |
| Related citations | |
| 5. | Autoimmun Rev. 2014 Dec;13(12):1167-73. doi: 10.1016/j.autrev.2014.08.022. Epub 2014 Aug 23.
Alunno A1, Carubbi F2, Bartoloni E1, Bistoni O1, Caterbi S1, Cipriani P2, Giacomelli R2, Gerli R3.
Author information:
Abstract
Compelling evidence suggests that the IL-17 axis plays a pivotal role in the pathogenesis of several autoimmune disorders including primary Sjögren's syndrome (pSS). However, although several studies have been carried out in experimental models and patients with pSS, many aspects of this field are not fully elucidated. In particular, the role played by different Th17 cell subsets as well as the effects of pharmacological therapies on IL-17 balance represent an intriguing issue. Furthermore, the understanding of IL-17 axis pathogenic role in pSS may be of interest for therapeutic purposes as a variety of compounds targeting IL-17, IL-17 receptor and other related cytokines and transcription factors involved in Th17 cell commitment are under intense investigation. The aim of this review article is to provide an overview of current knowledge in IL-17/Th17 cells in pSS and discuss their potential therapeutic targeting in this disease. Copyright © 2014 Elsevier B.V. All rights reserved. |
| PMID: 25183242 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 6. | BMC Res Notes. 2014 Aug 29;7:580. doi: 10.1186/1756-0500-7-580.
Author information:
Abstract
BACKGROUND:
Clinical complications of Sjoegren's syndrome include myelitis and skin manifestations. There is scarce observational data and a lack of randomised controlled studies regarding the treatment of Sjoegren's syndrome in the presence of such complications. CASE PRESENTATION:
Here we report the case of a 41-year-old Caucasian female patient with biopsy-proven Sjoegren's syndrome who initially presented with generalized exanthema and subsequently developed acute extensive transverse myelitis. In view of the rapid deterioration we opted for an intensive treatment using a combination of corticosteroid pulse therapy, plasmapheresis and cyclophosphamide, which we later changed to rituximab. Under that treatment the skin manifestations resolved entirely whereas transverse myelitis showed incomplete remission. CONCLUSION:
Severe neurological and dermatological complications may occur in Sjoegren's syndrome. This suggests a close yet currently unclear pathogenetic relationship. Intensive immunosuppressant treatment resulted in significant improvement of both symptom clusters. Skin manifestations may precede other severe complications in Sjoegren's syndrome and therefore require particular attention. |
| PMID: 25167870 [PubMed - indexed for MEDLINE] | |
| Related citations | |
  |
| 7. | Curr Opin Rheumatol. 2014 Sep;26(5):520-7. doi: 10.1097/BOR.0000000000000096.
Author information:
Abstract
PURPOSE OF REVIEW:
Primary Sjögren's syndrome is a systemic autoimmune disease whose clinical spectrum extends from sicca syndrome to systemic involvement (extraglandular manifestations). Recent reports have focused on expanding the clinical characterization and improving the diagnostic and therapeutic management of systemic Sjögren's. RECENT FINDINGS:
The development of the EULAR-SS disease activity index represents a step forward in the evaluation of systemic Sjögren's, and three multicenter studies including more than 2500 European patients have confirmed that primary Sjögren's syndrome is, undeniably, a systemic autoimmune disease. Systemic involvement plays a key role in the prognosis of primary Sjögren's syndrome, and recent studies have focused on cutaneous, pulmonary, renal and neurological disease features. Other studies comparing the two sets of Sjögren's syndrome criteria (American College of Rheumatology vs. American-European Consensus Group) in real-life patients found a moderate level of agreement. Autoantibodies are clues to an early diagnosis, as positivity confirms an autoimmune origin of the sicca syndrome and may appear several years before the disease diagnosis. In patients with a high clinical suspicion and negative results for the standard determination of anti-Ro/SS-A antibodies, specific detection of anti-Ro52/60 antibodies is recommended. Direct and indirect B-cell blocking seems to be the most promising biological pathway in primary Sjögren's syndrome, especially for systemic involvement, although a large controlled trial has failed to demonstrate the efficacy of rituximab for nonsystemic symptomatology (dryness, fatigue and pain). SUMMARY:
Dryness of the mucosal surfaces is the pivotal, but not only, clinical involvement that characterizes primary Sjögren's syndrome. There is growing interest in and knowledge of the clinical characterization and therapeutic management of systemic Sjögren's. |
| PMID: 25050925 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 8. | Curr Opin Rheumatol. 2014 Sep;26(5):528-37. doi: 10.1097/BOR.0000000000000084.
Author information:
Abstract
PURPOSE OF REVIEW:
To provide an update on infections in systemic lupus erythematosus (SLE) and Sjögren's syndrome, particularly addressing their role as triggers of autoimmunity, their impact on mortality, the main microorganisms, the approaches to differential diagnosis with disease flares and recommendations for vaccination. RECENT FINDINGS:
New mechanisms for autoimmunity triggered by Epstein-Barr virus and human commensal microbiota have been described. The increased risk for tuberculosis was recently demonstrated for the first time in Sjögren's syndrome. C-reactive protein was reported to be a more sensitive and specific marker for bacterial infections in SLE than procalcitonin and phagocyte-specific S100A8/A9 protein. Inactivated vaccines are well tolerated and efficacy was demonstrated for influenza vaccine. Immunogenicity is generally reduced but adequate in SLE. Prednisone or immunosuppressants are associated with decreased vaccine serological response, whereas hydroxicloroquine seems to improve vaccine immunogenicity. Other infection-preventive measures for these diseases include antimalarials and prophylaxis for tuberculosis or Pneumocystis jirovecii. SUMMARY:
Advances in the role of infectious agents as triggers for SLE and Sjögren's syndrome have provided new insights into disease development. Knowledge on vaccine immunogenicity, safety and efficacy has improved with evidence of a generally reduced but adequate response for inactivated vaccines in SLE. Other preventive measures comprise infection prophylaxis and antimalarials. |
| PMID: 25022358 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 9. | BMJ Case Rep. 2014 Jun 18;2014. pii: bcr2014204339. doi: 10.1136/bcr-2014-204339.
Ben Ghorbel I1, Litaiem N2, Chelly I3, Houman H1.
Author information:
Abstract
A 27-year-old woman presented with persistent dryness of the mouth and eyes. She presented with permanent photodistributed rash involving the face and distal extremities. Laboratory tests showed positive Sjögren's syndrome (SS)-A and SS-B antibodies. Histological examination of minor salivary gland biopsy revealed inflammatory infiltration grade 4 according to Chisholm's classification. Skin biopsy showed acanthosis, hyperkeratosis in the epidermis and little inflammatory infiltrate in the dermis. There was an infiltration of CD4 T lymphocytes in the dermis. Based on the characteristics of the dermatitis and on a rapid response to niacin replacement, the diagnosis of pellagra was carried out. A complete resolution of the dermatological signs was obtained within 2 months. To the best of our knowledge, the association between primary SS and pellagra has never been reported. We emphasise the possible mechanisms of this association. 2014 BMJ Publishing Group Ltd. |
| PMID: 24943141 [PubMed - indexed for MEDLINE] | |
| Related citations | |
| 10. | Cont Lens Anterior Eye. 2014 Oct;37(5):363-7. doi: 10.1016/j.clae.2014.05.005. Epub 2014 Jun 8.
Author information:
Abstract
PURPOSE:
A study was designed to evaluate the efficacy of three different strategies aiming at increasing spontaneous eyeblink rate (SEBR) during computer use. METHODS:
A total of 12 subjects (5 female) with a mean age of 28.7 years were instructed to read a text presented on a computer display terminal during 15min. Four reading sessions (reference and three "blinking events" [BE]) were programmed in which SEBR was digitally recorded. "Blinking events" were based on either a slight distortion of the text characters or on the presentation of a white screen instead of the text, with or without accompanying blinking instructions. All BE had a duration of 20ms and occurred every 15s. Participants graded the intrusiveness of each BE configuration, and the number of lines participants read in each session was recorded. RESULTS:
Data from 11 subjects was analysed. A statistically significant difference in SEBR was encountered between the experimental configuration consisting on a white screen plus blinking instructions (7.8 blinks/min) and both reference (5.2 blinks/min; p=0.049) and white screen without blinking instructions (4.8 blinks/min; p=0.038). All three BE had superior levels of intrusiveness than reference conditions, although the performance of participants (line count) was not compromised. CONCLUSIONS:
The joint contribution of white screen and blinking instructions has been shown to result in a short term improvement in blinking rate in the present sample of non-dry eye computer users. Further work is necessary to improve the acceptance of any BE aiming at influencing SEBR. Copyright © 2014 British Contact Lens Association. Published by Elsevier Ltd. All rights reserved. |
| PMID: 24917262 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 11. | J Dermatol. 2014 May;41(5):463-4. doi: 10.1111/1346-8138.12475.
Author information:
|
| PMID: 24801928 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 12. | Intern Med. 2014;53(7):783-7. Epub 2012 Mar 1.
Author information:
Abstract
This report describes a patient with autoimmune myelofibrosis accompanied by Sjögren's syndrome (SS). A 36-year-old woman was admitted due to petechiae, purpura, gingival bleeding, dyspnea on exertion, and a lack of concentration. She had pancytopenia and was diagnosed with SS. A bone marrow study showed hypercellular marrow with reticulin fibrosis. Lymphocytic infiltrates and aggregates composed of a mixture of T and B cells in the marrow were also observed. A chromosomal analysis of the marrow cells showed 47, XXX and an analysis of peripheral lymphocytes revealed 47, XXX/46, XX mosaic results. The patient's cytopenia resolved following treatment with oral prednisolone. |
| PMID: 24694497 [PubMed - indexed for MEDLINE] | |
| Related citations | |
 |
| 13. | Ann Rheum Dis. 2015 Mar;74(3):526-31. doi: 10.1136/annrheumdis-2013-203991. Epub 2013 Dec 17.
Mariette X1, Seror R1, Quartuccio L2, Baron G3, Salvin S2, Fabris M4, Desmoulins F1, Nocturne G1, Ravaud P3, De Vita S2.
Author information:
Abstract
BACKGROUND:
Increased expression of B cell activating factor (BAFF or B lymphocyte stimulator) may explain the B cell activation characteristic of primary Sjögren's syndrome (pSS). OBJECTIVES:
To evaluate the efficacy and safety of belimumab, targeting BAFF, in patients with pSS. METHODS:
Patients were included in this bi-centric prospective 1-year open-label trial if they fulfilled American European Consensus group criteria, were anti-Sjögren's syndrome A-positive and had current systemic complications or salivary gland enlargement, or early disease (25% improvement in any B cell activation biomarker values. RESULTS:
Among 30 patients included, the primary end-point was achieved in 18 (60%). The mean (SD) European League Against Rheumatism (EULAR) Sjögren's Syndrome Disease Activity Index decreased from 8.8 (7.4) to 6.3 (6.6) (p=0.0015) and EULAR) Sjögren's Syndrome Patient Reported Index from 6.4 (1.1) to 5.6 (2.0) (p=0.0174). The mean dryness, fatigue and pain VAS varied from 7.8 (1.8) to 6.2 (2.9) (p=0.0021), 6.9 (1.8) to 6.0 (2.2) (p=0.0606) and 4.6 (2.6) to 4.7 (2.4) (p=0.89), respectively. Salivary flow and Schirmer's test did not change. CONCLUSIONS:
These encouraging results justify future randomised controlled trials of belimumab in a selected target population of pSS patients most likely to benefit from treatment. Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://group.bmj.com/group/rights-licensing/permissions. |
| PMID: 24347569 [PubMed - indexed for MEDLINE] | |
| Related citations | |
| 14. | Arthritis Res Ther. 2012 Nov 29;14(6):R260. doi: 10.1186/ar4105.
Abstract
INTRODUCTION:
The aim of this study was to examine whether circulating levels of the pro-inflammatory glycoprotein tenascin-C (TNC) are elevated in musculoskeletal disorders including rheumatoid arthritis (RA) and to assess in RA whether levels are related to clinical disease status and/or patient response to treatment. METHODS:
TNC in serum or plasma was quantified by ELISA. Samples from 4 cohorts of RA patients were examined and compared to normal human subjects and to patients with other inflammatory diseases. RESULTS:
Circulating TNC levels were significantly raised in patients with RA, as well as patients with systemic lupus erythematosus, idiopathic inflammatory myositis, psoriatic arthritis and ankylosing spondylitis, whilst patients with Sjogren's syndrome displayed levels similar to healthy controls. The highest levels of TNC were observed in RA patients with late stage disease. In early disease TNC levels correlated positively with ultrasound determined erosion scores. Treatment of early RA patients with infliximab plus methotrexate (MTX) resulted in a transient decrease in circulating TNC over the first year of therapy. In contrast, TNC levels increased over time in RA patients receiving MTX alone. In patients treated with infliximab plus MTX, baseline TNC levels significantly correlated with tender joint counts (TJC) at 18 and 54 weeks after initiation of infliximab therapy. CONCLUSIONS:
|




/http%3A%2F%2Fstorage.canalblog.com%2F71%2F95%2F1309572%2F108183439_o.jpg)
/http%3A%2F%2Fstorage.canalblog.com%2F76%2F77%2F1309572%2F107960382_o.jpg)
/http%3A%2F%2Fstorage.canalblog.com%2F58%2F96%2F1309572%2F107815430_o.gif)
/http%3A%2F%2Fstorage.canalblog.com%2F12%2F26%2F1309572%2F107805770_o.jpg)